Neuropsychiatric Lupus
Lupus may affect the central nervous system in possibly up to 40% of those living with SLE. Often labelled by the rather scary sounding name, “neuropsychiatric lupus,” its symptoms can range from mild brain fog and headaches to more serious conditions like memory loss, seizures, strokes and others that can dramatically affect quality of life. Yet, knowing the symptoms and treatment options of neuropsychiatric lupus can truly be empowering – making this difficult form of lupus much more manageable! Read on to find out how!
- What is neuropsychiatric lupus?
- What can cause or trigger NPSLE?
- What are the symptoms of NPSLE?
- How is NPSLE diagnosed?
- What are the treatment options for NPSLE?
- In Conclusion
What is neuropsychiatric lupus?
Neuropsychiatric lupus, or neuropsychiatric SLE (NPSLE), is a form of lupus that affects both the central nervous system (the brain and spinal cord) and peripheral nervous system (everything else!). It can lead to neurological and psychiatric symptoms, such as impaired thinking, mood swings, and emotional difficulties that add problems to an already challenging disease. It is an incredibly complex form of lupus that varies from mild and often temporary symptoms to ones that are more severe, life-changing or even life-threatening!
It is difficult to study neuropsychiatric lupus. It, like lupus itself, can resemble many other conditions. However, there are some things we do know:
- It can affect between 30% and 50% of those living with lupus – though defining NPSLE is tricky and statistics vary widely among studies!
- It commonly develops in the early stages of lupus – over half in the first year of a diagnosis.
- It occurs more frequently in women, though seizures are more common in men.
- It affects Black and Asian patients than Whites, yet the severity of symptoms is generally higher in White patients.
What can cause or trigger NPSLE?
As with lupus in general, the fundamental causes of NPSLE are not known. However, research has discovered a few possible pathways. For example, the brain can be affected by lupus when inflammation or central nervous system vasculitis occurs in the brain’s blood vessels. It might also develop if lupus autoantibodies directly damage the blood-brain barrier. It is also thought that some autoantibodies can enter the cerebral spinal fluid and attack brain tissue itself. No one knows for sure.
In spite of this, there are some known risk factors for neuropsychiatric lupus:
- Genetics: Several genes that have been linked with NPSLE. So, as with lupus itself, certain people may be genetically predisposed to developing neuropsychological SLE.
- Hormones: In particular, estrogen is clearly associated with a higher risk for both lupus and neuropsychiatric lupus.
- Environmental triggers: These include sun exposure, certain drugs, viral infections, smoking tobacco and stress. Again, these are similar triggers for many other forms of lupus.
What are the symptoms of NPSLE?
NPSLE is extremely variable. Its effects can be very mild, or they can be quite serious … even life-threatening,
When SLE affects the brain and spinal cord, it can cause several symptoms:
- Brain fog is very common and a characteristic condition of lupus. It can manifest many other different symptoms, such as mild memory loss, confusion, difficulty concentrating or expressing thoughts. Notably, severe dementia is quite rare.
- Headaches are also common. Those that are associated with NPSLE, sometimes called “lupus headaches,” often do not improve with over-the-counter medications.
- Anxiety and depression are also relatively common, leading to a rapid heart beat, shaking, sweating and irritability.
- Seizures are not uncommon, affecting between 7% to 20% of those with NPSLE, particularly in men.
- Strokes can occur due to lupus autoantibody “complexes” that form blood clots (thromboses) in the brain.
- Insomnia and restless sleep are very common and can create a vicious cycle of increasing emotional problems.
- Rarely, psychotic episodes may occur, including hallucinations.
One of the worst aspects of neuropsychiatric lupus is the unpredictability of these symptoms. This can understandably lead to frustration, increased anxiety, and a constant fear of not knowing what each day will bring.
Finally, it is important to remember that some of these symptoms may be caused by lupus without direct involvement of autoantibodies attacking the central nervous system. Many of these symptoms can be also caused by conditions other than lupus. Some, including insomnia and mood problems, may result from the long-time use of certain lupus mediations, such as corticosteroids.
How is NPSLE diagnosed?
Neuropsychiatric lupus is a particularly difficult form of lupus to diagnose. There are no specific blood tests, biomarkers (though that may change soon!) or even CT or MRI imaging scans that, by themselves, can provide a clear diagnosis of NPSLE.
So, how can a person tell whether their confusion and emotional difficulties are really caused by lupus and are not just the result of the anxiety and stress that comes from living with any chronic, debilitating disease like SLE?
For now, the most common strategy is to eliminate all of the other possible causes for each symptom first. Then, lupus itself might be the most reasonable diagnosis. This takes time and may require:
- Neurological and psychiatric tests to evaluate a person’s mental functions;
- Sampling cerebral-spinal fluid (by lumbar puncture), to look for infections and autoantibodies;
- Electroencephalogram (EEG) studies to identify unusual brain activity, and
- MRI scans, which can image blood flow around the brain and reveal blood clots (which may be caused by lupus) and other vascular problems.
This takes a collaborative approach of neurologists, mental health therapists and others to work together as part of a patient’s lupus healthcare team.
What are the treatment options for NPSLE?
Since there is no cure for lupus or NPSLE, and because there are multiple ways that lupus can affect the brain and nervous system, the main strategy is to treat each cognitive and emotional symptom individually … while also treating the underlying lupus. Each person’s neuropsychiatric lupus will be different. So, adding to the possible hydroxychloroquine, anti-inflammatories (NSAIDs and steroids), and immunosuppressants that may be prescribed, treatment plans may also include:
- Emotional, behavioral and cognitive therapies;
- Antiepileptic drugs to treat seizures;
- Antidepressants and antianxiety medications;
- Anti-hypertension medications and anticoagulants to treat high blood pressure and to reduce the risk of blood clots in the brain;
- Anti-psychotic drugs if serious psychiatric symptoms are involved.
This seems like a lot … and it is! Yet, research in this area is growing quickly and hopefully, in the future, specific biologics and other medications will be able to directly treat the root causes of both lupus itself and NPSLE.
.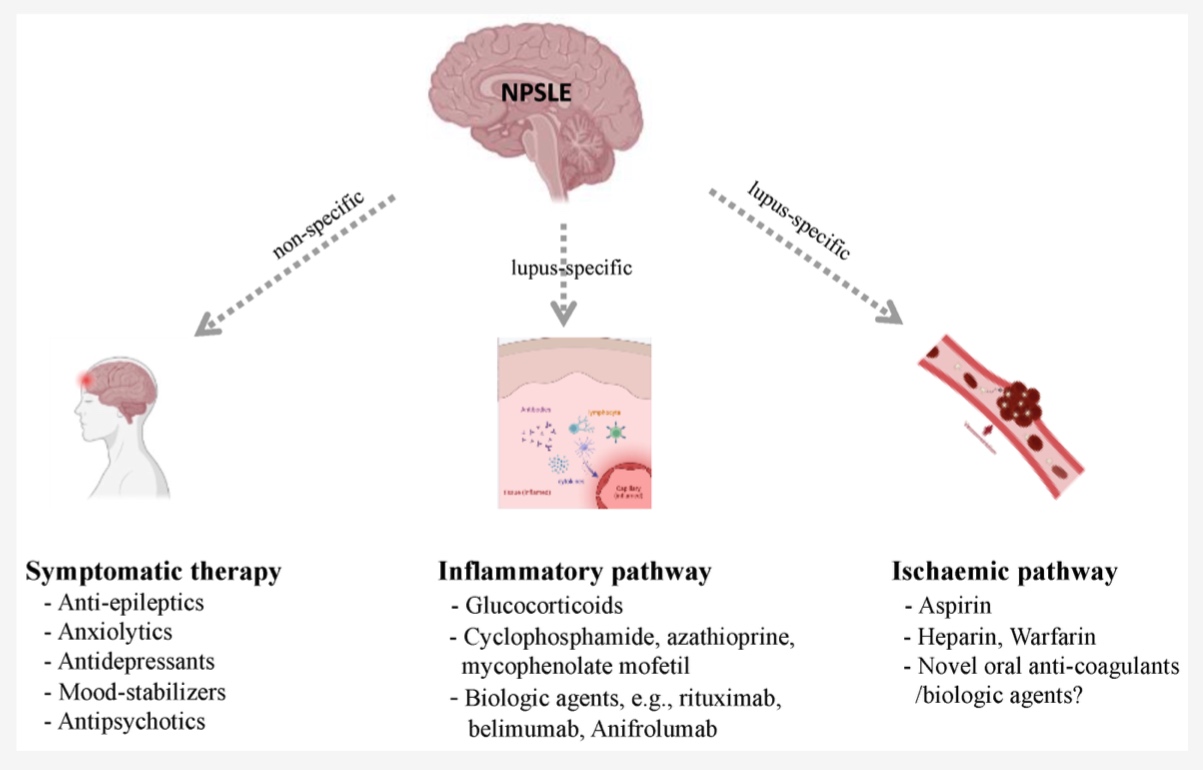
Diagram adapted from peer-reviewed article 10.3390/jcm11174955
In Conclusion
Neuropsychiatric lupus is a very complex form of SLE, which is itself a very complex condition already … yet there are plenty of reason for hope! There is a growing understanding of the mental and emotional consequences for those living with lupus – whether or not NPSLE is really the cause. This means that, more than ever, there are a growing number of mental health resources for everyone with SLE to use. Make sure you advocate for yourself and ask for the help you need!
Additionally, lupus research on NPSLE biomarkers is growing quickly, and the clinical trials of entirely new, more targeted medications will almost certainly mean better treatments in the future.
Finally, whether you suffer from neuropsychiatric lupus or not, your mental health is as important as your physical health. Ask for help if you need it. You are not alone!
For more information on lupus and the nervous system, check out these Kaleidoscope Fighting Lupus articles:
Peripheral Neuropathy and Lupus
Isolation and Anxiety: Living with Lupus
Dealing With a Lupus Depression: How Do You Cope?
.
References
Cincinnati Children’s. (2023, July 20). Neuropsychiatric systemic lupus erythematosus (NPSLE) in children.Cincinnati Children’s Health Library. https://www.cincinnatichildrens.org/health/n/neuropsychiatric-systemic-lupus-erythematosus
Gelfand, J.M., & Yazdney, J. (2023, July 20). Neurologic and neuropsychiatric manifestations of systemic lupus erythematosus. UpToDate. https://www.uptodate.com/contents/neurologic-and-neuropsychiatric-manifestations-of-systemic-lupus-erythematosus
Hanly JG, Li Q, Su L, et al. (2019). Psychosis in systemic Lupus Erythematosus: results from an International Inception Cohort Study. Arthritis Rheumatology, 71(2), 281–289.
Kirou, K.A., & Ruiz, R.F. (2023, July 14). Neuropsychiatric Lupus: Lupus and the Brain. Hospital for Special Surgery. https://www.hss.edu/conditions_neuropsychiatric-sle-lupus-and-brain.asp
Kivity, S., Agmon-Levin, N., Zandman-Goddard, G., Chapman, J., & Shoenfeld, Y. (2015). Neuropsychiatric lupus: a mosaic of clinical presentations. BMC Medicine, 13. Article number 43. https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-015-0269-8
Lindblom, j., Mohan, C., & Parodis, I. (2022). Biomarkers in neuropsychiatric systemic lupus erythematosus: A systematic literature review of the last decade. Brain Sciences, 12(3), 192. https://doi.org/10.3390/brainsci12020192
Marcello, G. (2020). 20 Diagnosis and treatment of neuropsychiatric lupus. Lupus, 7(2). http://dx.doi.org/10.1136/lupus-2020-la.20
Sarwar, S., Mohamed, A.S., Rogers, S., Sarmast, S.T., Kataria, S., Mohamed, K.H., Khalid, M.Z., Saeeduddin, M.O., Shiza, S.T., Ahmad, S., Awais, A., & Singh, R. (2021). Neuropsychiatric systemic lupus erythematosus: A 2021 update on diagnosis, management, and current challenges.Cureus, 13(9), e17969. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8516357/
Wang M, Wang Z, Zhang S, Wu Y, Zhang L, Zhao J, Wang Q, Tian X, Li M, & Zeng X. (2022). Progress in the pathogenesis and treatment of neuropsychiatric systemic lupus erythematosus. Journal of Clinical Medicine, 11(17), 4955. https://doi.org/10.3390/jcm11174955
.
Author: Greg Dardis, MS
Professor Dardis was the Chair of the Science Department at Marylhurst University and is currently an Assistant Professor at Portland State University and the American College of Healthcare Sciences. His focus has been human biology and physiology with an interest in autoimmunity. Professor Dardis is also a former President of the Board of Directors of Kaleidoscope Fighting Lupus.
All images unless otherwise noted are property of and were created by Kaleidoscope Fighting Lupus. To use one of these images, please contact us at [email protected] for written permission; image credit and link-back must be given to Kaleidoscope Fighting Lupus.
All resources provided by us are for informational purposes only and should be used as a guide or for supplemental information, not to replace the advice of a medical professional. The personal views expressed here do not necessarily encompass the views of the organization, but the information has been vetted as a relevant resource. We encourage you to be your strongest advocate and always contact your healthcare practitioner with any specific questions or concerns.



 .
.