New Protocol for Diagnosing Lupus
The American College of Rheumatology’s (ACR), in 1997, approved a specific set of criteria for the diagnosis of systemic lupus erythematosus (SLE). Recently, however, in collaboration with the European League Against Rheumatism (EULAR), these criteria have been significantly revised. Read on to learn more about these important changes and how they can affect how lupus is diagnosed.
Introduction
The ACR’s classification criteria for SLE have been used worldwide as a cornerstone for determining the diagnosis of lupus, yet it had not been revised in over 20 years. As research and clinical studies advanced, there was a need to have a more interdisciplinary and international approach to lupus diagnosis, and to develop more specific and sensitive ways to classify the most important criteria. In response, the ACR collaborated with EULAR to develop new criteria that include a weighted system for calculating the probability of the presence of SLE as opposed to other systemic autoimmune disease such as Sjögren’s syndrome. It can be difficult to differentiate between those two diseases using the 1997 ACR criteria, for example, as both diseases often and significantly overlap each other.
A 1999 article published in the journal Lupus discussed the need for change and the evolution of classification criteria over time in order for that information to “reflect and facilitate a better understanding of the disease.” At that time, researchers of the 1999 article recommended the following for future classification revisions:
- The revisions should include individuals who were originally diagnosed with SLE, but would not meet the criteria in future studies.
- They should place as much value on the degree of symptoms, organ involvement and damage, disease duration and activity as on the number of criteria met or unmet.
- The periodical revision of criteria should at some point include a simple weighted system that “may more accurately reflect clinical practice.”
These recommendations were used to inform a new study that would look into revising the outdated criteria.
What needed to change?
Several lupus research centers across Europe worked on this international initiative, with the ACR and EULAR, to analyze the existing criteria and write new ones. According to Dr. Jack Cush of RheumNow – Rheumatology News and Information the study was conducted in four phases:
- Assessing the feasibility of including antinuclear antibody (ANA) as new criteria. Researchers analyzed several databases that included over 13,000 individuals from several studies and found a 97.8% ANA sensitivity, convincing researchers of the necessity of ANA inclusion in the new classification.
- Determining how to reduce criteria. The number of criteria was reduced from 43 to 21. This simplified things, but also included differentiating between “required” criteria – those that were absolutely necessary for a lupus diagnosis – and others called “additive” criteria.
- Discussing how to define and weigh new criteria. A group of SLE patient advocates, a steering committee and international SLE experts collectively determined how to redefine and weigh the final reduced list of criteria through “[achieving] consensus on classifying a case vignette as SLE.”
- Deciding how to refine weighting and threshold scores with a new cohort of subjects. Experts determined a “data-driven threshold for classification” and evaluated information on individuals thought to have SLE but who were below the threshold and “misclassified” against individuals who unequivocally had SLE yet still missed classification requirements. Experts again refined the proposed weighing system, rounding the weights to whole numbers, according to the findings from their evaluation. A steering committee “unanimously endorsed” the new system.
The new classification reflects the “largest international, collaborative SLE classification effort to date.” Twenty-three international lupus research centers engaged in this study and subsequent revisions, each selecting individuals with SLE and those without to partake in the research. A group of 1,001 individuals were reviewed using the proposed new criteria while a group of 1,270 individuals were reviewed using existing criteria in order to compare the difference in diagnoses from one set of criteria to the other.
According to an article published in the September 2019 issue of Annals of the Rheumatic Diseases, the study took place in the Department of Rheumatology, Hopitaux Universitaires Paris Sud, which is a reference center for “rare systemic autoimmune disease.”

What are the significant changes from 1999 to 2020 criteria?
Dr. Cush notes the following significant changes to the new criteria:
-
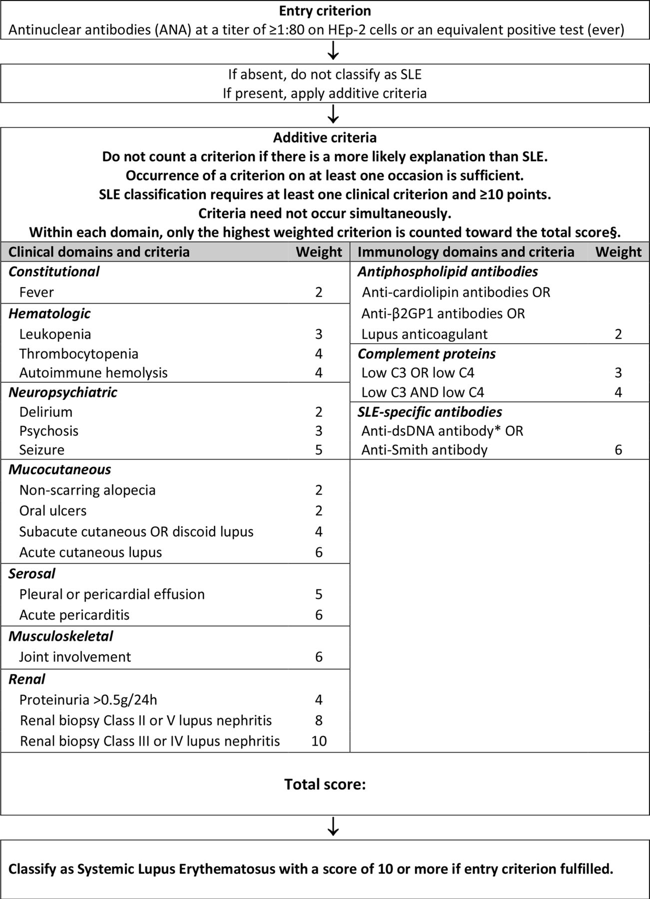
- Criteria is chosen from seven clinical categories including: constitutional, hematologic, neuropsychiatric, mucocutaneous, serosal, musculoskeletal and renal.
- Criteria is chosen from three immunologic categories including: antiphospholipid antibodies, complement proteins and SLE-specific antibodies.
- Criteria is weighted from two to ten.
- Derivation and validation sensitivity and specificity percentages have increased from the previous criteria.
- Individuals with ≥ 10 points are classified as having SLE.
The 1997 classification outlined 11 criteria that are common to SLE. If an individual met at least 4 of the criteria, the likelihood was high that they had SLE, prompting their healthcare practitioner to perform additional tests and create treatment plans based on the analysis. Researchers of the 2019 study published in the journal Annals of the Rheumatic Diseases note that the new criteria was developed with “multidisciplinary and international input,” and has “excellent sensitivity and specificity.”
New EULAR/American College of Rheumatology Classification Criteria for SLE
The following is the new SLE EULAR/ACR classification criteria:
A supplement to this new classification gives specific examples of how the new rating system works in diagnosing an individual with SLE. The examples show a practical application of the new system in order to understand how it works. The following is an excerpt from the supplement that puts the rating system into practice to give a clearer picture of its use:
30 year female patient with new onset polyarthritis. Anti-CCP antibodies negative, no erosions on plain x-ray films, Hep-2 ANA 1:320 (homogenous), anti-dsDNA antibodies positive in ELISA and verified by CLIFT (Crithidia luciliae immunofluorescence test)
Entry criterion: Fulfilled (ANA ever positive by Hep-2 ≥1:80 or equivalent test)
Clinical criterion: Fulfilled (Joint involvement): 6 points
Attribution to SLE: Correct (Anti-CCP is negative, no more likely cause of arthritis)
Lupus specific antibody: anti-dsDNA positive (CLIFT has ≥90% proven specificity against relevant disease controls, ELISA anti-dsDNA alone usually not): 6 points
ANA entry + 12 points: This patient should be classified as having SLE.

In Conclusion
This new classification may seem confusing and overwhelming at first. We strongly suggest speaking with your trusted healthcare practitioner about these changes and if they will affect your diagnosis and treatment. Learning as much as you can about the new system will prepare you to advocate for yourself and other individuals with lupus who may be confused or scared about what these changes may mean. Rest assured that researchers have your best interests at heart – this study and resulting classification update “reflect current thinking about SLE and provide an improved foundation for SLE research.”
References
1997 Update of the 1982 American College of Rheumatology Revised Criteria for Classification of Systemic Lupus Erythematosus. (n.d.). Retrieved from: https://www.rheumatology.org/Portals/0/Files/1997%20Update%20of%201982%20Revised.pdf
2019 European League Against Rheumatism/American College of Rheumatology Classification Criteria for Systemic Lupus Erythematosus (n.d.). [Patient examples using 2019 EULAR/ACR classification criteria]. Retrieved from: https://www.rheumatology.org/Portals/0/Files/Classification-Criteria-Systemic-Lupus-Erythematosus-Supplement-2.pdf
Aringer, M., Costenbader, K., Daikh, D., Brinks, R., Mosca, M., Ramsey-Goldman, R., … Johnson, S., (2019). 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Arthritis & Rheumatology. Retrieved from: https://ard.bmj.com/content/annrheumdis/78/9/1151.full.pdf
Cush, J. (2019). New EULAR/ACR classification criteria for SLE. RheumNow. Retrieved from: http://rheumnow.com/content/new-eularacr-classification-criteria-sle
European League Against Rheumatism/American College of Rheumatology. (n.d.). [Table of 2019 EULAR/ACR Classification Criteria for SLE]. Annals of Rheumatic Diseases. Retrieved from: https://ard.bmj.com/content/annrheumdis/78/9/1151/F2.large.jpg
New 2019 SLE EULAR/ACR classification criteria are valuable for distinguishing patients with SLE from patients with pSS. (2019). Annals of the Rheumatic Diseases. Retrieved from: https://ard.bmj.com/content/annrheumdis/early/2019/09/09/annrheumdis-2019-216222.full.pdf
ORGENTEC Diagnostika. (2013, April 28). Autoimmunity Blog [digital image]. Retrieved from http://autoimmunityblog.com/
Smith, E. & Shmerling, R. (1999). The American College of Rheumatology criteria for the classification of systemic lupus erythematosus: Strengths, weaknesses, and opportunities for improvement. Lupus. Retrieved from: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.861.4441&rep=rep1&type=pdf
Author: Liz Heintz
Liz Heintz is a technical and creative writer who received her BA in Communications, Advocacy, and Relational Communications from Marylhurst University in Lake Oswego, Oregon. She most recently worked for several years in the healthcare industry. A native of San Francisco, California, Liz now calls the beautiful Pacific Northwest home.
All images unless otherwise noted are property of and were created by Kaleidoscope Fighting Lupus. To use one of these images, please contact us at [email protected] for written permission; image credit and link-back must be given to Kaleidoscope Fighting Lupus.
All resources provided by us are for informational purposes only and should be used as a guide or for supplemental information, not to replace the advice of a medical professional. The personal views expressed here do not necessarily encompass the views of the organization, but the information has been vetted as a relevant resource. We encourage you to be your strongest advocate and always contact your healthcare practitioner with any specific questions or concerns.

