Lupus and Autoimmune Hypophysitis
The pituitary is the most important endocrine gland in your body and autoimmune hypophysitis, though rare, is a condition that can dramatically affect your health and your life with lupus. How? Read on to find out!
- The 30-second Overview
- Your Pituitary – A Quick Overview
- Autoimmune Hypophysitis – A Quick Overview
- Autoimmune Hypophysitis and Lupus
- So what you can do?
- In Conclusion
.
The 30-second Overview
Autoimmune hypophysitis (AH) is a chronic inflammation of the pituitary gland. It can be serious because, even though it is only about the size of a pea, the pituitary is your “master gland.” Your pituitary not only produces several important hormones that regulate body functions, but it also controls the functioning of many other glands and the hormones they produce.
Autoimmune hypophysitis is considered rare, but it is increasingly being diagnosed, and research is finding more connections between it and other autoimmune conditions, like lupus.
Here are the basics:
- Autoimmune hypophysitis (AH) is also called lymphocytic hypophysitis because it is often diagnosed when the pituitary is filled with lymphocytes – white blood cells that attack the gland during the autoimmune response.
- Symptoms include headaches, nausea, vomiting, changes to your visual field, diabetes insipidus and a higher than normal production of the hormone prolactin.
- AH affects both males and females though is significantly higher in pregnant women. In one study over 40% of the women with AH were also pregnant.
- Autoimmune hypophysitis can complicate a diagnosis of lupus – or vice versa – because both have overlapping autoimmune-related symptoms.
- Luckily, they can be treated with similar pharmaceuticals and both can reach remission.
- Some studies have shown that the excess prolactin associated with AH can aggravate lupus disease activity.
- About 2% of those with autoimmune hypophysitis also have lupus.
Want to know more? Let’s start by exploring the pituitary gland in more detail.
Your Pituitary – A Quick Overview
The pituitary is the most important endocrine gland in the body. It sits at the base of the skull, and is intimately connected to the hypothalamus of the brain. It is only about the size of a pea, but its structure and functions are surprisingly complex.
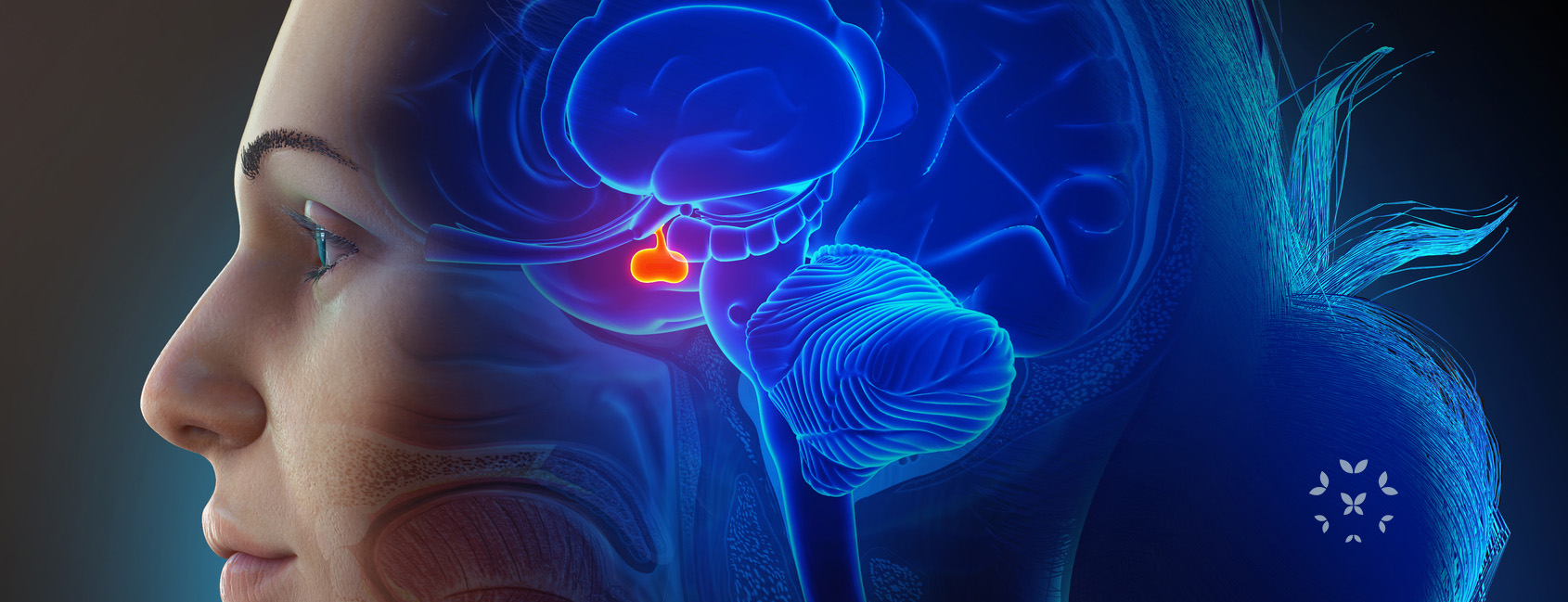
As an endocrine gland, it stores and produces several hormones that it releases to the blood stream, some of which in turn influence other endocrine glands and their hormones. That is why it is called the “master gland.” It influences or controls an incredible number of body functions, such as appetite, thirst, sweating, narrowing of blood vessels of the skin, the body’s metabolism and growth, reproductive cycles and more.
Some of the hormones it produces can also influence lupus and the health of those living with SLE. These include:
- Adrenocorticotropic hormone (ACTH), which regulates the production of cortisol, your body’s primary stress hormone.
- Thyroid-stimulating hormone (TSH), which stimulates your thyroid, the gland that is critical for the T cells that are so important in the autoimmune response.
- Growth hormone (GH), which stimulates muscle and bone growth.
- Follicle-stimulating hormone (FSH), which induces the ovaries to produce estrogen.
- Luteinizing hormone (LH), which stimulates ovulation by the ovaries and testosterone production by the testes.
- Vasopressin or antidiuretic hormone (ADH), produced by the hypothalamus and released by the pituitary, it regulates water balance in the body and kidney function.
- Prolactin, a hormone that stimulates breast milk production but also influences the levels of estrogen and testosterone in both men and women.
It is this last hormone, prolactin, that is notably affected by autoimmune hypophysitis and, in turn, may affect lupus.

Autoimmune Hypophysitis – A Quick Overview
Causes: In autoimmune hypophysitis, the body’s immune system attacks all or parts of the pituitary gland causing chronic inflammation. This is similar to the damage lupus can cause to other organs of the body. Autoantibodies against the pituitary gland creates inflammation and cause the pituitary to enlarge and turn a grey/yellow color as it swells with an unhealthy number of lymphocytes. As the pituitary enlarges, it loses its ability to function and produces a number of symptoms.
Symptoms include:
- Headaches and changes to the visual field are classic first indications of AH, as the swelling of the pituitary gland puts pressure on specific parts of the brain.
- Nausea and vomiting.
- Dramatic increase in thirst and urination (diabetes insipidus) caused by the decrease in vasopressin, the hormone that helps regulate your body’s water balance.
- Hyperprolactinemia, a higher than normal production of prolactin, can affect the reproductive system and the levels of estrogen and testosterone in both women and men.
.
Diagnosis: The diagnosis of AH can be pretty challenging because so many symptoms, such as headaches and nausea are associated with many other conditions. Blood tests can find changes in some hormone levels (like prolactin) that may indicate AH, but again, those may have other causes. More specific tools include:
- Blood tests that are for specific autoantibodies of the pituitary. However, these are rarely ordered.
- Magnetic resonance imaging (MRI) can detect enlargement of the pituitary, but that can be indicative of other pituitary conditions.
- A pituitary biopsy is usually the only way to get a definitive diagnosis.
.
Treatment:
- Hormone replacement is a common therapy, especially for sex hormone imbalances, depending upon specific symptoms.
- Anti-inflammatories, especially corticosteroids, which can help with counteract the loss of adrenal gland function.
- Immunosuppressive drugs, like azathioprine and methotrexate can reduce the inflammatory response as it does for lupus.
- Autoimmune hypophysitis has also been known to spontaneously resolve itself.
Autoimmune Hypophysitis and Lupus
The relationships among lupus, AH and the pituitary are still unclear. However, there are some important factors to consider:
- Lupus is not known to directly cause autoimmune hypophysitis.
- About 2% of those with AH also have lupus.
- Autoimmune hypophysitis may trigger lupus activity.
- Some studies have shown that the excessive production of prolactin with AH increase lupus disease activity. This happens through a complex domino effect of hormones. First, the pituitary produces prolactin, the hormone that promotes breast milk production during pregnancy. Excessive prolactin can also throw off levels of estrogen and this has been implicated in triggering lupus – particularly during pregnancy.
- An increased production of prolactin is found in 20%-30% of those with lupus, though rarely is it caused by autoimmune hypophysitis.
So what you can do?
Again, autoimmune hypophysitis is rare. However, there are so many possible connections with lupus, and they share similar symptoms and treatment plans.
Here is a good list of things to keep in mind:
- Stay on your treatment plan and let your healthcare provider know of any changes in the state of your lupus.
- If you are pregnant or planning to be pregnant, be aware of any possible changes in symptoms that might indicate the onset of autoimmune hypophysitis.
- Maintain a healthy (perhaps anti-inflammatory) diet and eat foods rich in the omega 3’s and 6’s, which can be found in salmon, halibut, walnuts, cashews and avocados
- Avoid as much as possible, junk food! Too much refined sugar, salt and processed foods can affect pituitary or other glands of your endocrine system.
- Be careful of supplements that claim to improve your endocrine system.
- Try to be as physically active as possible. This can mean walks and low impact workouts like yoga. Don’t push yourself too hard, but keep moving! Physical activity can positively affect the feedback loops within the endocrine system!
- Reduce stress! Make sure to get 7-8 hours of sleep each night, try meditation, breathing exercises, and calm or repetitive activities like walking, knitting, etc.
In Conclusion:
Living with lupus can mean dealing with a number of other unexpected and complex conditions like autoimmune hypophysitis. AH is relatively rare, however there is growing evidence for how it relates to SLE and other autoimmune conditions … and this may lead to future diagnostic tools and treatments. The more you learn about your pituitary gland and the possible symptoms that might indicate AH, the better you can communicate with your healthcare providers to ensure you are following the best treatment plan. As with lupus, there is no cure for autoimmune hypophysitis. However, both can be treated successfully and remission may be possible!
References
Bellastella, G., Maiorino, M. I., Bizzarro, A., Giugliano, D., Esposito, K., Bellastella, A., & De Bellis, A. (2016). Revisitation of autoimmune hypophysitis: Knowledge and uncertainties on pathophysiological and clinical aspects. Pituitary, 19(6), 625–642. https://doi.org/10.1007/s11102-016-0736-z
Caturegli, P. Newshaffer, C. Olivi, A., Pomper, M.G., Burger, P.C., & Rose, N.R. (2005). Autoimmune hypophysitis. Endocrine Reviews, 26(5). 599-614. https://doi.org/10.1210/er.2004-0011
Ji, J.D., Lee, S.Y., Choi, S.J., Lee, Y.H., & Song, G.G. (2000). Lymphocytic hypophysitis in a patient with systemic lupus erythematosus. Clinical and Experimental Rheumatology,(18), 78-80.
Joshi, M.N., Whitelaw, B.C., & Carroll, P.V. (2018). Mechanisms in endocrinology: Hypophysitis: Diagnosis and treatment. European Journal of Endocrinology, 179(3). R151-R163. https://doi.org/10.1530/EJE-17-0009
Kapur, S., Oswal, J.S., Jahagirdar, R., & Viswanathan, V. (2021) Autoimmune hypophysitis in systemic lupus erythematosus. Indian Pediatrics, 58(1) 84-85. DOI:10.1007/s13312-021-2106-9
Langlois, F., Varlamov, E. V., & Fleseriu, M. (2022) Hypophysitis, the growing spectrum of a rare pituitary disease. The Journal of Clinical Endocrinology & Metabolism, 107(1). 10-28. https://doi.org/10.1210/clinem/dgab672
Li, J., May, W., & McMurray, R.W. (2005). Pituitary hormones and systemic lupus erythematosus. Arthritis & Rheumatism, 52I(12). 3683-4052. https:doi.org/10.1002/art.21436
Nadira, U., Cader, R. A., Kong, N. C., Mohd, R., & Gafor, H. A. (2012). Systemic lupus erythematosus with a non functioning pituitary macroadenoma. The American Journal of Case Reports, 13, 160–162. https://doi.org/10.12659/AJCR.883248
Xiang, P., Wu, Q., Zhang, H., Luo, C., & Zou, H. (2020). Autoimmune hypophysitis with systemic lupus erythematosus: A case report and literature review. Frontiers in Endocrinology, (11). Article 579436. https://doi.org/10.3389/fendo.2020.579436
Yoshihara, R., Tsuchiya, H., Tsuzuki, S., Harada, H., Shoda, H., & Fujio, K. (2021). Hypophysitis identified on initial presentation of systemic lupus erythematosus: A case report and review of the literature. Scandinavian Journal of Rheumatology, 50(5), 413-415. DOI: 10.1080/03009742.2020.1861648
Author: Greg Dardis, MS
Professor Dardis was formerly the Chair of the Science Department at Marylhurst University and is currently an Assistant Professor at Portland State University. His focus has been human biology and physiology with an interest in autoimmunity.
All images unless otherwise noted are property of and were created by Kaleidoscope Fighting Lupus. To use one of these images, please contact us at [email protected] for written permission; image credit and link-back must be given to Kaleidoscope Fighting Lupus.
All resources provided by us are for informational purposes only and should be used as a guide or for supplemental information, not to replace the advice of a medical professional. The personal views expressed here do not necessarily encompass the views of the organization, but the information has been vetted as a relevant resource. We encourage you to be your strongest advocate and always contact your healthcare practitioner with any specific questions or concerns.


