Lupus and the Eyes
Up to one-third of individuals with lupus will develop some form of eye complications. Learning about the signs, symptoms and treatment options can help maintain the health of your delicate eyes.
- Introduction
- A Brief Anatomy of the Eye
- What eye diseases may affect an individual with lupus?
- What causes eye disease in individuals with lupus?
- Maintaining Good Eye Health
- In Conclusion
.
Introduction
There is an old saying that goes, “the eyes are the windows to the soul.” While the eyes can communicateemotion and feeling, they can also convey health. Healthcare practitioners treating lupus may use the eyes as diagnostic tool that may indicate an SLE flare, disease progression and changes in health due to drug therapy. The eyes of individuals with lupus can also be extremely vulnerable to illness and disease, making regular exams and checkups imperative to monitoring and maintaining overall health and well-being.
Authors of a review published in the journal Rheumatology found that approximately 10% of individuals with SLE may develop some form of retinal disease ranging from mild, asymptomatic retinopathy to more severe conditions that may result in vision loss if not treated early and properly. We rely on our eyes for almost everything we do. So, it is imperative for an individual with lupus to understand what conditions may arise and how to protect their eyes and keep them healthy.
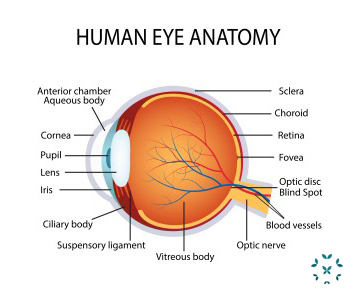
A Brief Anatomy of the Eye
The structures that support, protect and surround the eyes include:
- The orbit: The bony socket where each eye sits.
- The extraocular muscles: These six muscles attach the orbit to the eye.
- The lacrimal gland: The gland that produces the watery part of tears.
- The meibomian gland: The gland that produces the oily part of tears.
- The tear duct: The tears made from the lacrimal and meibomian glands drain through the tear ducts.
- The conjunctiva: The conjunctiva is the membrane that covers the lining of the eyelids.
The front of the eye includes:
- The sclera: the white part of the eye made of strong connective tissue.
- The cornea: the transparent, dome-shaped front part of the eye that not only forms the surface of the eye, but also bends even before it reaches the lens. The general term for inflammation of the cornea is “keratitis.”
- The iris: the colored part of the eye.
- The pupil: the opening in the middle of the iris that allows light to reach the back of the eye.
- The lens: the lens sits behind the pupil and focuses light and changes shape as it focuses.
The structures found at the back of the eye include:
- The choroid: The pigmented, vascular part of the eye between the sclera and retina.
- The retina: The light-sensitive tissue that lines the back of the eye.
The optic nerve: The retina communicates to the brain through the optic nerve.
What eye diseases may affect an individual with lupus?
Eye diseases occurring as a result of lupus that may affect the structures that support, protect and surround the eye include:
- discoid lupus or discoid-like rashes of the eyelids;
- conjunctivitis, chronic inflammation of the conjunctiva which commonly results in “pink eye;”
- lacrimal system disease such as dry eye syndrome (keratoconjunctivitis sicca) and secondary Sjögren’s syndrome; and
- rarer diseases including orbital myositis, vasculitis, panniculitis, periorbital edema and orbital masses.
Eye diseases occurring as the result of lupus that may affect the front of the eyeball itself include:
- corneal diseases including corneal erosion, peripheral corneal infiltration, ulcerative keratitis, interstitial keratitis and endotheliosis;
- episcleral and scleral disease which can both be presenting features of SLE as the sclera (the white outer layer of the eyeball) becomes inflamed causing irritation and pain;
- anterior uveitis which causes inflammation in the middle eye and usually occurs with episcleral or scleral disease and rarely by itself;
- Adie’s pupil which causes the pupil dysfunction and even the iris to change color;
- retrochiasmal disease or disorders of the visual pathway; and
- transient monocular blindness or temporarily impaired vision or blindness in one eye or the other.
Eye diseases occurring as the result of lupus that may affect the structures of the back of the eye and the retina include:
- Choroidal disease, which causes dystrophy of the choroid blood vessels of the eye. Scientists believe that this condition is underdiagnosed in lupus and is the most responsible for sight loss in SLE.
- Retinopathies (diseases of the retina) including hypertensive retinopathy, vasculitis and artery/vein occlusion.
- Occurring in approximately 10% of individuals with SLE, an individual with retinopathy tends to see spots, “floaters,” have blurred vision or difficulty perceiving colors.
- Retinal Spasms or retinal vasospasms can occur in which there is cyclical filling and emptying of the retinal vessels – sometimes called a retinal Raynaud’s like phenomenon – that usually involves just one eye.
- Also very rarely, SLE eye conditions can mimic retinal migraines that can cause brief blindness in one eye during a migraine headache.
Retinal complications may occur in between 7 – 26% of individuals around the age of 25 who have lupus. Scientists believe that lupus retinopathy “may even be the harbinger of a potentially severe systemic flare-up” and an indication that a current treatment plan may no longer be working adequately.
There may also be a link between renal dysfunction such as lupus nephritis and retinopathy. In a small study of 91 individuals with SLE, researchers found that all of the individuals in the study who had renal impairment also had retinopathy. While it is unclear what the link is, researchers think that retinopathy may develop in more severe SLE, which is also when renal complications may develop.
Eye diseases occurring as the result of lupus that may affect the nerves to and from the eyes include:
- optic neuritis and optic neuropathy which occur when there is inflammation of or damage to the myelin protective sheath around the optic nerve and the nerve itself;
- Horner’s syndrome which results when there is damage to the sympathetic nerves of the face causing the upper eyelid to drop and the pupil to improperly function;
- light-near disassociation which occurs when the pupil’s ability to respond to light is impaired, but otherwise functions properly; and
- idiopathic intracranial hypertension which occurs when pressure inside the skull increases and mimics a brain tumor. The pressure from swelling can damage the optic nerve.
While ocular nerve involvement occurs in only about 1% of individuals with lupus, eye movement disorders which cause abnormal eye alignment and difficulty controlling the eyes may occur in up to 29% of individuals with SLE and may involve both the brain and the muscles that control eye movement.
It is important to report any eye discomfort and symptoms of the above conditions immediately to a healthcare practitioner. While seasonal allergies, environmental irritants and the need for corrective lenses may be to blame, it is imperative to seek medical attention in order to rule out – or treat – some of the more serious conditions listed as soon as possible.
What causes eye disease in individuals with lupus?
Eye problems can be triggered by the following:
- Autoimmune disease and inflammation: Individuals with pre-existing autoimmune disease or a family history of it may be more at risk for developing eye problems.
- Hydroxychloroquine: An adverse reaction to chronic treatment with hydroxychloroquine (Plaquenil) has been known to cause conditions such as cataract, photophobia, extraocular muscle palsy and anterior uveitis. Between 0 – 4% of individuals who take hydroxychloroquine may also experience toxic retinopathy.
- Corticosteroid therapy: Ironically, some of the drugs used to treat lupus can actually cause problems including elevated eye pressure, cataract and eye infections. In a small study of 170 individuals with lupus, researchers found that 29% of the individuals who were routinely taking corticosteroids developed cataracts and 3% developed glaucoma, both with an earlier onset than the general population.
- Diabetes: Individuals with lupus who also have diabetes are at greater risk of developing eye diseases including glaucoma, diabetic retinopathy and even blindness.
- Antiphospholipid syndrome (APS): An eye condition may be the initial presenting factor in an individual who has not been previously diagnosed with Approximately 80% of individuals with APS will have eye involvement. Eye conditions that have been reported include optic-neuropathy retinal vein thrombosis, retinal artery thrombosis and retinal vascular occlusion.
- Hypertension: Hypertension can cause a form of retinopathy. Individuals with the eye condition are also at a 35% increased risk of stroke.
Other conditions that may cause eye problems include: poor vision, injury, allergies and illnesses such as the common cold or flu.
Scientists have also found immune complexes that are unique to the eye. The antibodies that are typically present include antiphospholipid antibodies (APA) and antineuronal antibodies (ANA). APA is often present with severe retinopathy and vascular occlusions.
Diagnosing and Treating Eye Conditions in Lupus
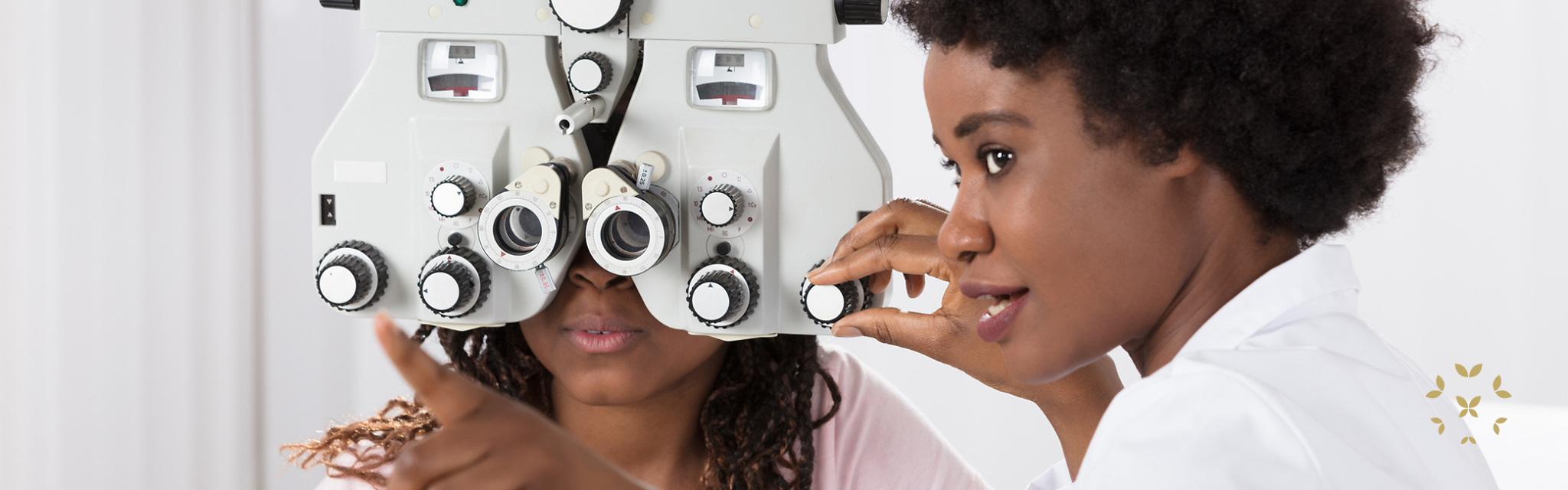
An ophthalmologist, optometrist and even a rheumatologist can work together to diagnose, treat and monitor eye health.
Initially, a complete eye exam will be completed by an ophthalmologist. Typically, these exams include:
- providing a complete medical and symptom history including any past and present eye problems;
- eye muscle tests that measure how well the muscles of the eyes function;
- a visual acuity test that determines the need for prescriptive lenses;
- a refraction test that looks at how light passes through to the back of the eye;
- a visual field test that determines how well an individual sees in their complete field of vision;
- color vision testing that looks for color-blindness;
- a glaucoma screening that measures pressure inside the eye after numbing drops and dye are administered;
- an exam that assesses the overall health and function of the eyes (front, inside, optic nerve and retina) that is given after dilating drops are administered; and
- other tests as necessary including scans and/or biopsies.
Once the eye condition is properly diagnosed, it may be treated with the following:
- prescriptive lenses to correct vision issues;
- artificial tears;
- steroidal eye drops;
- systemic immunosuppressive therapy including methylprednisolone, cyclophosphamide, azathioprine,methotrexate, ciclosporin or mycophenolate;
- topical corticosteroids;
- biologics such as rituximab that are effective for treating retinal vasculitis and also improve vision;
- laser therapy or surgery to correct a detached retina and retinopathy; and
- anticoagulants and acetylsalicylic acid (low-dose aspirin) to treat some forms of retinal disease and ophthalmic disease, particularly when an individual has APS.
Maintaining Good Eye Health
Maintaining good eye health not only takes a team of healthcare practitioners, but the individual with lupus as well. There are several steps that can be taken on a regular basis to maintain and improve eye health and protect vision:
- Get complete eye exams as recommended by a healthcare practitioner.
- Maintain a health and symptom history.
- Work to keep blood pressure at a healthy level. Learn ways to reduce stress and manage anxiety. Seek mental health therapy if the fear and anxiety become overwhelming.
- Take care of overall health through exercise, proper nutrition, maintaining a healthy weight and not smoking. Limit alcohol and sugar intake.
- Ask a healthcare practitioner if there are any vitamins or supplements to take that support eye health.
- Wear sunglasses (even on the cloudy days) that are polarized and block 99 – 100% of damaging UV rays.
- Wear glasses and/or contacts as prescribed to avoid eyestrain.
- Wear glasses that protect eyes from the blue-light emitted by electronic devices.
- Take contacts out and replace as often as recommended, keeping them disinfected.
- Wear protective eye gear when playing sports, doing hobbies or home repairs.
- Give eyes a rest! Our eyes work hard and need to relax. Take a break from looking at screens every 20 minutes when working, studying, watching videos or gaming.
- If there is a concern about eye health risk, ask. Self-advocate by openly and honestly discussing concerns with a healthcare practitioner.
Your eyes provide insight into both your emotional and physical well-being and should be treated as the precious and valuable organs they are. Scheduling regular eye exams, seeking urgent medical help when new symptoms occur, understanding the side-effects from medications and staying on top of eye health away from the practitioner’s office can help to protect and preserve sight for years to come. Remember, for those with lupus, there are ways to prevent and treat the eye damage that may occur. Don’t take your eye health for granted.
References
Carli, L., Tani, C., Querci, F., Rossa, A., Vagnani, S., Baldini, C., Talarico, R., d’Ascanio, A., Neri, R., Tavoni, A., Bombardieri, S., & Mosca, M. (2013). Analysis of the prevalence of cataracts and glaucoma in systemic lupus erythematosus and evaluation of the rheumatologists’ practice for the monitoring of glucocorticoid eye toxicity. Clinical Rheumatology, 1071-1073. doi: 10.1007/s10067-0130221406. Retrieved June 22, 2020 from https://link.springer.com/content/pdf/10.1007/s10067-013-2214-6.pdf
Common eye disorders and diseases. (2020). Centers for Disease Control and Prevention. Retrieved June 22, 2020 from https://www.cdc.gov/visionhealth/basics/ced/index.html
Eyes. (2020). Johns Hopkins Medicine. Retrieved June 22, 2020 from https://www.hopkinsmedicine.org/health/eyes
Eye exam. (2019). Mayo Clinic. Retrieved June 22, 2020 from https://www.mayoclinic.org/tests-procedures/eye-exam/about/pac-20384655#:~:text=During%20the%20exam,numbing%20drop%20in%20your%20eyes
Elvin, M. (2011, May 23). Eye problems in lupus. Hospital for Specialty Surgery. Retrieved June 22, 2020 from https://www.hss.edu/conditions_eye-problems-lupus.asp
Keeping your eyes healthy. (2020). National Eye Institute. Retrieved June 22, 2020 from https://www.nei.nih.gov/learn-about-eye-health/healthy-vision/keep-your-eyes-healthy
Kharel (Sitaula), R., Shah, D., & Singh, D. (2016). Role of lupus retinopathy in systemic lupus erythematosus. Journal of Ophthalmic Inflammation and Infection, 6(15), 1-4. doi: 10.1186/s12348-106-0081-4. Retrieved June 22, 2020 from https://joii-journal.springeropen.com/articles/10.1186/s12348-016-0081-4
Palejwala, N., Walia, H., & Yey, S. (2012). Ocular manifestation of systemic lupus erythematosus: A review of the literature. Autoimmune Disease. doi: 10.1155/2012/290898. Retrieved June 22, 2020 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3395333/#:~:text=Lupus%20choroidopathy%20with%20exudative%20retinal,well%20as%20uncontrolled%20blood%20pressure.
Parts of the eye. (2020). American Academy of Ophthalmology. Retrieved June 22, 2020 from https://www.aao.org/eye-health/anatomy/parts-of-eye
Phatak, S., Jaison, J., Soman, M., Mohan, A., & Nair, R. U. (2020). Retinal vasospastic phenomenon in a known case of systemic lupus erythematosus. Indian journal of ophthalmology, 68(11), 2575–2577. https://doi.org/10.4103/ijo.IJO_161_20
Retinal detachment. (2019). Mayo Clinic. Retrieved June 22, 2020 from https://www.mayoclinic.org/diseases-conditions/retinal-detachment/diagnosis-treatment/drc-20351348
Shoughy, S. & Tabbara, K. (2016). Ocular findings in systemic lupus erythematosus. Saudi Journal of Ophthalmology, 117-121. Retrieved June 22, 2020 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4908056/pdf/main.pdf
Silpa-archa, S., Lee, J., & Foster, S. (2015). Ocular manifestations in systemic lupus erythematosus. British Journal of Ophthalmology, 135-141. doi: 10.1136/bjophthamol-2015-306629. Retrieved June 22, 2020 from https://www.smo.org.mx/archivos/smonline/british/articulos/135-141.pdf
Sivaraj, R., Durrani. O., Denniston, A., Murray, P., & Gordon, C. (2007). Ocular manifestations of systemic lupus erythematosus. Rheumatology, 46(12), 1757-1762. doi: 10.1093/rheumatology/kem173. Retrieved June 22, 2020 from https://academic.oup.com/rheumatology/article/46/12/1757/1788657
Tezuka T, Shibata M, & Hanaoka H. (2023). Systemic lupus erythematosus mimicking retinal migraine: a case report. Cephalalgia, 43(12). doi:10.1177/03331024231219477
The eyes and lupus. (n.d.). Lupus UK. Retrieved June 22, 2020 from https://www.lupusuk.org.uk/medical/gp-guide/clinical-aspects-of-lupus/the-eyes-and-lupus/
Author: Liz Heintz
Liz Heintz is a technical and creative writer who received her BA in Communications, Advocacy, and Relational Communications from Marylhurst University in Lake Oswego, Oregon. She most recently worked for several years in the healthcare industry. A native of San Francisco, California, Liz now calls the beautiful Pacific Northwest home.
All images unless otherwise noted are property of and were created by Kaleidoscope Fighting Lupus. To use one of these images, please contact us at [email protected] for written permission; image credit and link-back must be given to Kaleidoscope Fighting Lupus.
All resources provided by us are for informational purposes only and should be used as a guide or for supplemental information, not to replace the advice of a medical professional. The personal views expressed here do not necessarily encompass the views of the organization, but the information has been vetted as a relevant resource. We encourage you to be your strongest advocate and always contact your healthcare practitioner with any specific questions or concerns.