Lupus – B Cells, T Cells and the Immune System
When B cells and T cells don’t know when to quit – the result – is lupus. Both are specialized blood cells that are critical for a healthy immune system, but they also cause the damage that comes with lupus. Read on to learn more about how these cells are supposed to defend the body, how they run out of control with lupus, and yet they may provide the key to an eventual cure.
- An Introduction to Lupus and the Cells of Immunity
- B Cells and T cells in Lupus
- Therapies That Target B Cells and T Cells
- In Conclusion
.
An Introduction to Lupus and the Cells of Immunity
Our bodies have a large and diverse “army” of immunity cells called white blood cells or leukocytes. They come in many shapes and sizes. They can circulate in the blood stream, hangout in lymph nodes or find places throughout the body, waiting to be activated when an infection occurs. The two most important white blood cells in terms of autoimmunity – and specifically for lupus – are the B lymphocytes and T lymphocytes… or B cells and T cells for short.
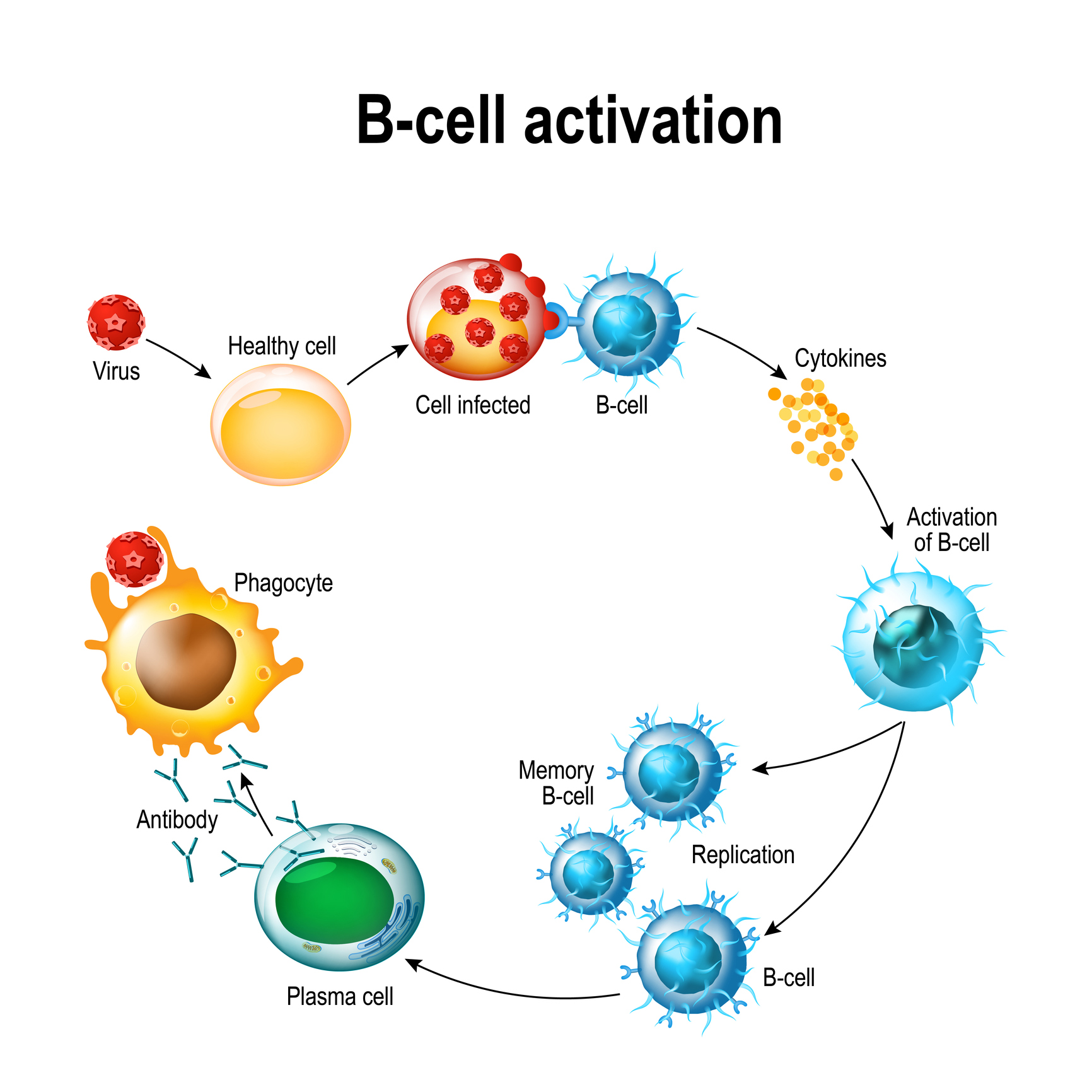
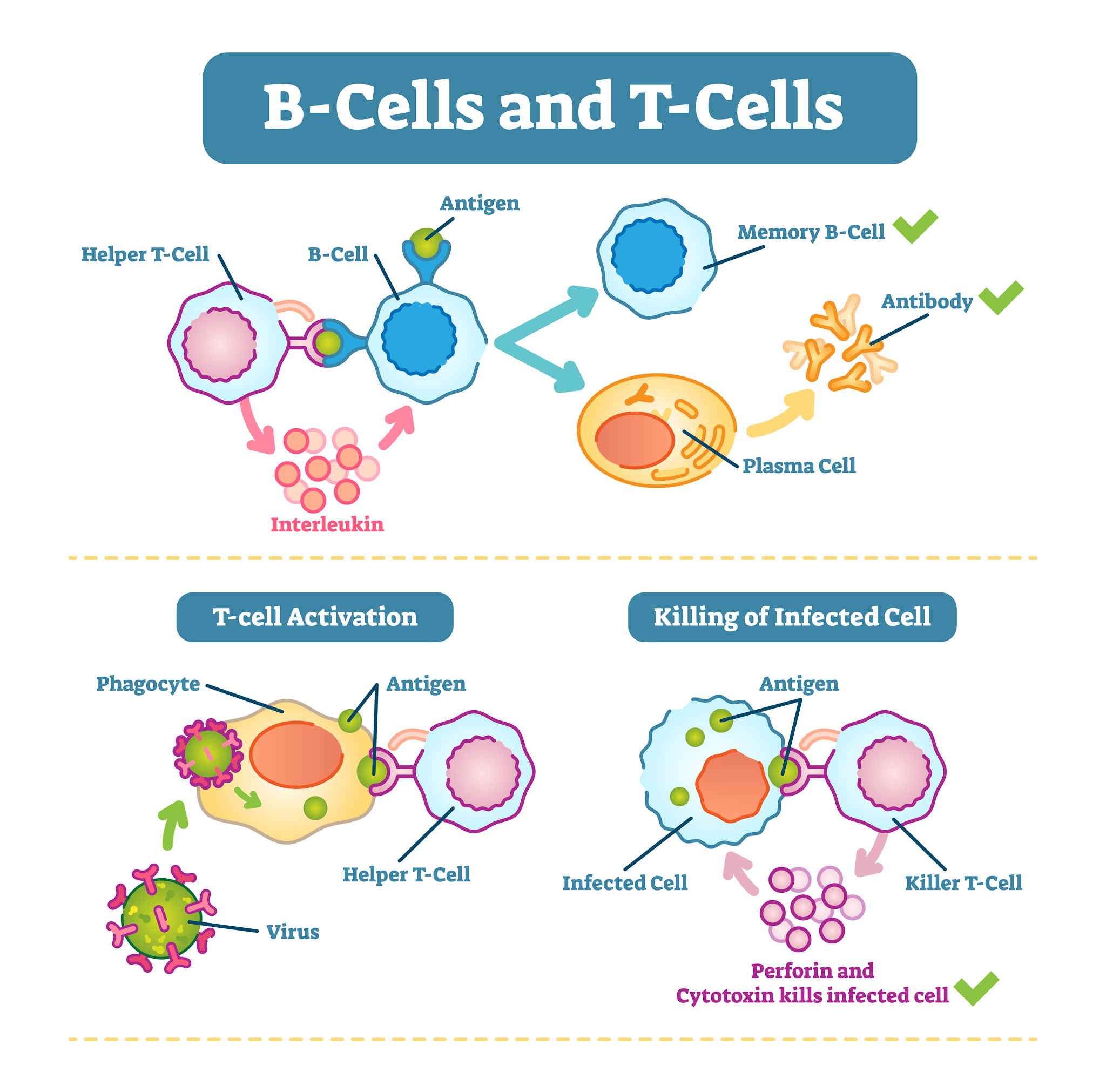
B cells are largely responsible for producing antibodies, the chemical weapons of the immune system. When the body recognizes an infection, some B cells become what are called plasma cells and produce antibodies – while others become memory B cells and wait for future infections . Unfortunately, in autoimmune diseases like lupus, some B cells produce autoantibodies, which attack the body’s own cells and tissues. The most diagnostic antibodies found in patients with lupus are the antinuclear antibodies (ANAs).
T cells are a bit more complicated. There are several types of T cells, and they have many functions, but the four most important with regards to lupus are: killer T cells, helper T cells, memory T cells, and regulatory T cells. Each has a role in the body’s immune response, and each is important in terms of its role in lupus. Recently, they have become the most important area of research for both the causes and possible treatments for lupus.
.
Here is a quick overview of those T cells:
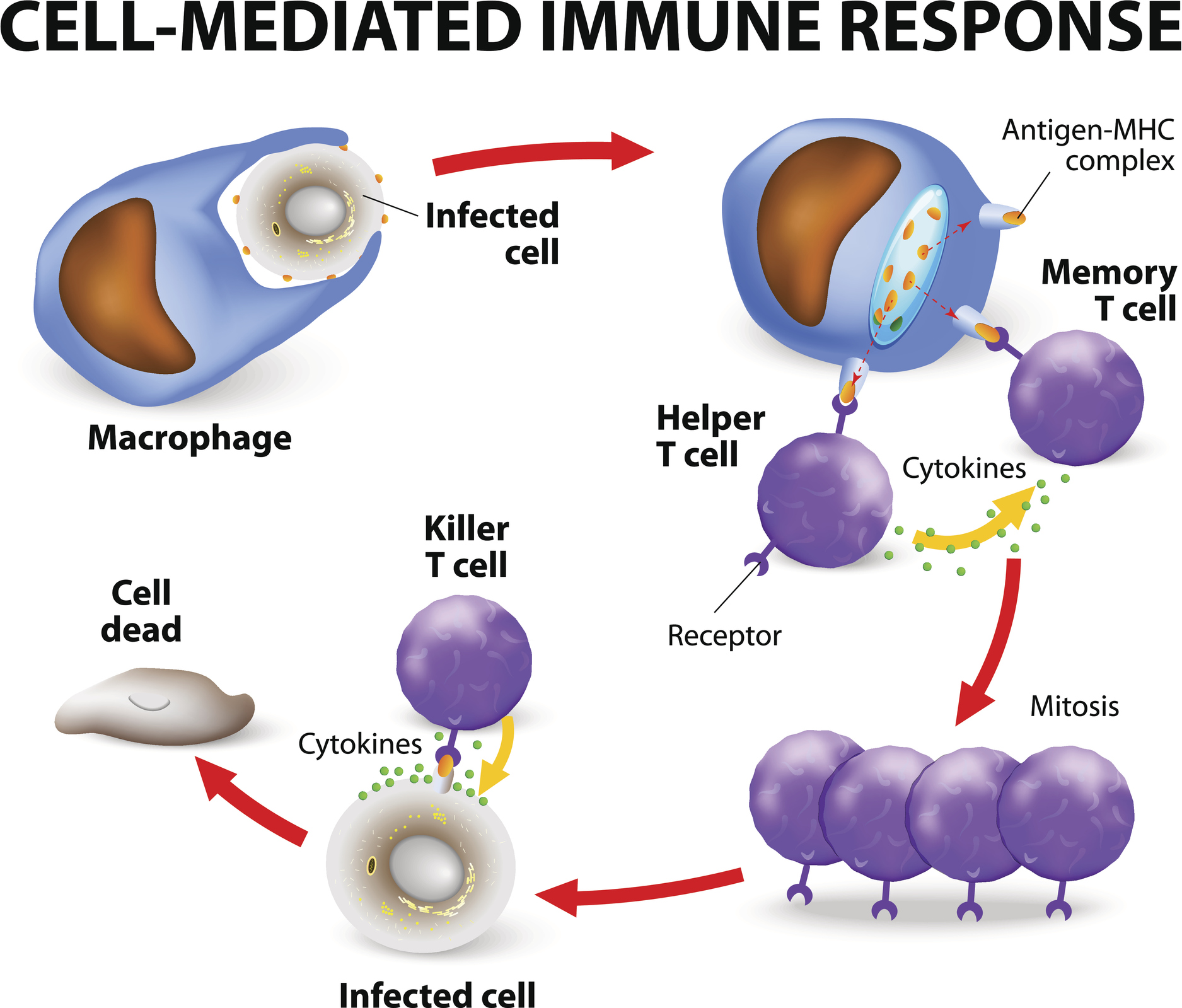
Helper T cells are the most numerous of the T cells. Their job is to “sound the alarm” and get other immune cells, like B cells, macrophages (large, microbe-eating white blood cells) and other T cells to activate the immune response. They do this by sending chemical signals called cytokines. The cytokines produced by helper T cells accelerate the immune response and inflammation. They have names that may be familiar to many lupus patients, such as interferon or the interleukins, because they are often the target of anti-inflammatory drug therapies or biologics.
Killer T cells (also called cytotoxic T cells), as their names imply, have the ability to find and destroy unhealthy or infected cells in the body. For example, they can recognize cells that are infected with viruses and eliminate them with special cytotoxins, like perforin (see diagram below). Amazingly, they can also recognize cancer cells, and get rid of them as well. Obviously, both of these are very helpful functions. However, if killer T cells go too far, they can mistakenly target and damage normal, healthy cells and that can lead to autoimmunity.
Memory T cells are special T cells that live long after an infection is over. They “remember” the infection by holding on to the antigens – the chemical identity of the virus, bacteria or parasite that was the source of infection. These memory T cells are important because they allow the immune system to recognize a previous infection and provide a faster response to subsequent infections.
Regulatory T cells, or Tregs, have the job of moderating or reducing the immune response. Their role is to slow down the body’s immune response after an infection is over. Tregs also help to suppress any autoreactive T cells from attacking the body’s own cells. In this way, regulatory T cells help manage what is called, self-tolerance, the condition that normally prevents autoimmune damage.
More Quick Facts about T cells:
- Memory T cells are the reason why vaccines work. They ”remember” the antigens contained in the vaccine and are ready to activate the immune system quickly in case of a future infection.
- T cells get their name from the fact that they must spend time in the thymus gland before they can begin their role in the immune system.
- In the thymus gland, they spend several days being trained and tested – almost like a ”boot camp“ for lymphocytes.
- Only about 2% of the T cells in the thymus survive the training and selection process to become mature T cells and part of the immune system.
- As people age, the thymus shrinks and the number of T cells it can produce is reduced. This partially accounts for why a person’s immune response slowly gets weaker with age.
- T cells are the immunity cells targeted by the HIV virus. When they are depleted enough, that can lead to AIDS.
.
B Cells and T cells in Lupus
Research has shown that the B cells and T cells of those with lupus act significantly different from those who do not have lupus. How? Here are some specifics:
- With lupus, B cells produce autoantibodies that attack healthy cells when activated by helper T cells. These autoantibodies, then, either directly attack the body’s own cells or indirectly damage organs by creating micro-blood clots (antibody-antigen complexes) and vasculitis in their capillaries – both can happen to the kidneys with lupus nephritis.
- Killer T cells themselves attack healthy cells and create so many pro-inflammatory cytokines that they amplify the inflammation reaction of other immune cells causing damage to the body’s own tissues and organs.
- Lupus patients can have too many autoreactive memory T cells. This keeps the immune system in a constant state of being oversensitive to the body’s own antigens and unpredictably initiate future inflammation reactions.
- Those with lupus generally have fewer regulatory T cells, so there are fewer Tregs to inhibit the autoimmune response and maintain self-tolerance.
.
Therapies That Target B Cells and T Cells
The more researchers learn about B cells and T cells, the more they have become focus of lupus treatments. Every year, new approaches to targeting the effects of these cells are learned. Here are just a few examples of the present and future therapies that specifically target B cells and T cells.
Belimumab (Benlysta), the first pharmaceutical specifically designed to treat lupus, is a monoclonal antibody (an antibody produced in a lab) that actually helps prevent B cells from producing the autoantibodies in lupus.
Hydroxychloroquine (HCQ), the antimalarial drug that is commonly prescribed to lupus patients has been found to interfere with how T cells over-activate the immune response. HCQ can block T cells from recognizing autoantigens and reduce the T cell’s ability to produce proinflammatory cytokines.
Voclosporin (Lupkynis), the first oral treatment for lupus nephritis approved by the FDA, is an immunosuppressant drug that specifically blocks helper T cells from producing the cytokine, Interleukin 2. This slows down the activation of killer T cells and the inflammation response.
CAR T Cells: Recently, there has been exciting research showing that it is may possible to develop a special kind of T cell, called a CAR T cell that is specifically designed to eliminate the B cells that produce autoantibodies. This therapy requires collecting the T cells of patients and genetically engineer them to attack the B cells that create the autoantibodies specific to that patient. This process creates chimeric antigen receptors (CARs) on these cells. These CAR T cells are then reintroduced into the patient. This technique has already proven successful with some forms of cancer and clinical trials on lupus patients have shown very promising results.
In 2023, the FDA fast tracked the designation for one of these therapies, called IMPT-514, to be approved for lupus and lupus nephritis patients! In that same year, a small German study reported that CAR T cell therapy resulted in all participants attaining remission and the elimination of autoimmune in SLE patients … while not affecting the immunity provided by their normal vaccinations. This is potentially game-changing news!
None of these therapies is a cure, but the research behind each one provides a glimpse into the lives of these cells that may one day lead to that cure.
.
In Conclusion
Lupus is a complex disease, largely because it affects so many diverse parts of an incredibly complex immune system. The more we learn about how B cells and T cells work, and how they are affected by lupus, the closer we get to understanding the causes of lupus and possibly its ultimate cure!
References
Compte, D., Karampetsou, M.P., & Tsokos, G.C. (2015) T cells as a therapeutic target in SLE. Lupus, 24(0), 351-363. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4372812/
How lupus affects the immune system. (n.d.) Johns Hopkins Lupus Center. Retrieved March 29, 2021, from https://www.hopkinslupus.org/lupus-info/lupus-affects-body/lupus-immune-system/
Janeway, C.A. Jr., Travers, P., & Walport, M. (2001) Generation of lymphocytes in bone marrow and thymus. Immunobiology: The Immune System in Health and Disease (5th ed.) Garland Science. https://www.ncbi.nlm.nih.gov/books/NBK27123/
Kansai, R., Richardson, N., Neeli, I., Shawaja, S., Chamberlain, D., Ghani, M., Ghani, Q.U., Balazs, L., Beranova-Giorgianni, S., Georgianni, F., Kachenderfer, J.N., Marion, T., Albritton, L.M., & Radic, M.(2019). Sustained B cell depletion by CD19-targeted CAR T cells is a highly effective treatment for murine lupus. Science Translational Medicine.11, 482-497.
Katsuyama, T., Tsokos, G.C., & Moulton, V.R. (2018). Aberrant T cell signaling and subsets in systemic lupus erythematosus. Frontiers in Immunology, 9, 1088–1088. https://doi.org/10.3389/fimmu.2018.01088
Mak, A., & Yee Kow, N. (2014). The pathology of T cells in systemic lupus erythematosus. Journal of Immunology Research, 2014, 419029-8. https://doi.org/10.1155/2014/419029
Mullard, A. (2023). CAR T cell therapies raise hopes — and questions — for lupus and autoimmune disease. Nature. https://www.nature.com/articles/d41573-023-00166-x
Sharabi, A., & Tsokos, G.C. (2020). T cell metabolism: new insights in systemic lupus erythematosus pathogenesis and therapy. Nature Reviews Rheumatology, 16, 100-112. https://doi.org/10.1038/s41584-019-0356-x
Schett, G., Munoz, L., Taubmann, J., Aigner, M., Bergmann, C., Knitza, J., Kroenke, G., Werner, D., Müller, F, & Mackensen, A. (2023, November 10-13). CAR T cell therapy leads to lang-term abrogation of autoimmunity in SLE patients while vaccination responses are maintained. [Poster session]. ACR Convergence 2024, San Diego, CA, United States.
Suarez-Fueyo, A., Bradley, S.J., & Tsokos, G.C. (2016). T cells in systemic lupus erythematosus. Current Opinions in Immunology, 43, 32-38. DOI:10.1016/j.coi.2016.09.001
Wallace, D.J. (2019) The lupus book: A guide for patients and their families. Oxford University Press.
Author: Greg Dardis, MS (Updated 2023)
Professor Dardis is the Chair of the Science Department at Marylhurst University, as well as, an Assistant Professor at Portland State University. His focus has been human biology and physiology with an interest in autoimmunity.
All images unless otherwise noted are property of and were created by Kaleidoscope Fighting Lupus. To use one of these images, please contact us at [email protected] for written permission; image credit and link-back must be given to Kaleidoscope Fighting Lupus.
All resources provided by us are for informational purposes only and should be used as a guide or for supplemental information, not to replace the advice of a medical professional. The personal views expressed here do not necessarily encompass the views of the organization, but the information has been vetted as a relevant resource. We encourage you to be your strongest advocate and always contact your healthcare practitioner with any specific questions or concerns.

